55 F with low back ache since 15 years
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-Centered online learning portfolio and your valuable inputs on the comment box is welcome."
CHEIF COMPLAINTS
55 year old female hailing from casba ,Assam belonging to the low socioeconomic status (acc modified BG Prasad scale ) came with the CHEIF complaints of lower back ache since 15 years .
HISTORY OF PRESENTING ILLNESS
Patient is a resident of casba,Assam married at the age of 18 years ,started working in farms 4 years after her marriage ,her work many consisted of ploughing ,sowing ,transplanting which requires her to bend foward and lean for long periods of time (5-10 hrs /day ) .She was apparently asymptomatic 15 years back when she developed low back ache ,which was insidious in onset and gradually progressive , radiating type ,to both the lower limbs more on left side ,more in the calf muscles ,associated with tingling and numbness more the the right side .Pain aggravates on sitting ,she is unable to sit for long durations, pain aggravated on coming back to standing position from bending foward ,on twisting the hips,extending backwards ,no relieving factors ,
Due to the progressive nature she stopped working in the fields 8 years back
patient had consulted a doctor in Kolkata 8 years back regarding the same ,was given injection at the SI joint ,after which she felt relief for 1-2 months ,later she developed similar complaints of low back ache
Patient also complaints of urinary urgency since 10 years ,not associated with burning micturation ,pain ,hestitancy ,frequency.
Patient also complaints of neck pain since 10 years associated with headache and she consulted a doctor regarding the same she received medication and few exercises which she religiously takes everyday but complaints of no relief from meds and exercises.
PAST HISTORY
K/c/o of Hypertension since 10 years
k/c/o cervical spondylisis since 8 years
Not a known case of DM,TB,epilepsy ,thyroid disorders ,trauma to the back ,major accidents .
MENSTRUAL HISTORY
Patient underwent hysterectomy 23 years back(35 years old )due to complaints of amenorrhea.
FAMILY HISTORY
No similar complaints in the family .
PERSONAL HISTORY
patient was married at the age of 18 years ,non consanguineous marriage,she did not receive any form of education ,started working in the farms 4 years after her marriage involving ploughing and sowing ,transplanting the sampling requiring her to bend foward and lean for several hours (5-10hrs/day)
She gave birth to her first child 2 years after marriage ,a male child
2 years after her first child she gave birth to second child ,female
2 years later she gave birth to her third child,female
Tubectomised 2 years after last birth
Underwent hysterectomy 10 years after tubectomy was done due to complaints of amenorrhea
Patient says she not her cheerful self due to the constant pains since 15 years
Patient also couldn’t sit outside without a fan even for few minutes ,complaints of hot flashes
diet -mixed
Appetite -normal
Sleep -disturbed due to low back pain
Bowel and bladder -complaint of urgency
addictions -started consuming tobacco (tamaka) after her marriage everyday ,in small quantities ,consumes till date .
no known allergies
TREATMENT HISTORY
k/c/o HTN since 8 years
Amlodopine 5 mg OD
SURGICAL HISTORY
tubectomised
hysterectomy done
GENERAL EXAMINATION
patient is coinscious coherent and co operative
Well oriented to time ,place ,person
Moderately built ,moderately nourished
Pallor -present in the lower palpebral conjunctiva
Icterus- absent
Cyanosis -absent
clubbing -absent
Lymphadenopathy -absent
Pedal edema -absent
VITALS
TEMP -afebrile
PULSE RATE -86bpm
PULSE PRESSURE -120/80mmHg
RESPIRATORY RATE -16cpm
SYSTEMIC EXAMINATION
CVS
Elliptical & bilaterally symmetrical chest
-No visible pulsations/engorged veins on the chest
-Apex beat seen in 5th intercostal space medial to mid clavicular line
-S1 S2 heard
-No murmurs
RESPIRATORY SYSTEM
Upper respiratory tract normal
Lower respiratory tract :
-Trachea is central
-Movements are equal on both sides
-On percussion resonant on all areas
-Bilateral air entry equal
-Normal vesicular breath sounds heard
-No added sounds
-Vocal resonance equal on both sides in all areas
CNS
Higher mental functions
-Patient is conscious, coherent,co-operative.Oriented to time, place,person.
-Speech = Fluency,comprehension,repetition intact
-Memory =Recent,Remote,Immediate : Intact
Cranial nerve examination -
other cranial nerves are normal
Motor examination :
Bulk of muscle normal on both sides on inspection
Tone
Right. Left
Upper limb. Normal. Normal
Lower limb. Normal. Normal
POWER
upper limbs +5 in all proximal and distal muscles
Lower limbs
Rt LT
Iliopsoas- +5 +5
Adductor femoris +5 +5
Gluteus medius +5 +5
And minimus
STRAIGHT LEG RASING TEST
patient complaints of pain on raising leg 90* on rt and 70 * on left from horizontal
It is a diffuse type of low back pain ,non radiating with tingling sensation in both the lower limbs more on the left side
Pain aggravated on Dorsiflexion of foot along with leg raising
Right. Left
Biceps. ++ ++
Triceps. + + ++
Supinator. + +. ++
Knee. + +. ++
Ankle. + +. ++
Plantar. flexor flexor
Sensory examination:
1.Spinothalamic: R L
Crude touch + +
Pain + +
tingling sensation in both the lower limbs
2.Posterior column:
Fine touch + +
Vibration Normal
Position sense- normal
3.Cortical
Stereognosis: + +
Graphesthesia +. +
CEREBELLUM:
Finger nose and finger finger test were normal
No dyadiadokokinesia
No pendular knee jerk
Heel knee test : normal
PER ABDOMEN EXAMNATION
-Scaphoid
-No visible pulsations/engorged veins/sinuses
-Soft,non tender, no guarding and rigidity, no organomegaly
-Bowel sounds heard
IMPRESSION:
Lumbar spondylosis with degenerative disc disease at L3/14 to L5/SI levels showing diffuse disc bulge causing ventral thecal sac indentation at all levels, AP central canal stenosis at L5-SI level. bilateral neural foraminal stenosis at all levels and indentation of right L5 traversing nerve
root.
MRI CERVICAL SPINE
PLAIN
IMPRESSION:
Cervical spondylosis with degenerative disc disease at C5/C6 disc level showing focal left paracentral disc bulge causing ventral thecal sac indentation and impingement of left C6 nerve root at root - exit zone.
MRI day-4 (29-04-2023)
On 26-04-2023(day-1)
Day-2
TREATMENT :(day-1)
This is a case of a 53-year-old female with lumbar spondylosis. The patient is having sleep disturbances and is taking tablet heel cam plus since five years for sleep at bedtime. The patient is habituated to take medications frequently for unknown complaints. Patient is referred to us in view of further evaluation,
history of presenting illness,
patient was apparently alright around 15 to 20 years ago, then one fine day, she noticed having constant back pain (lower) and with passing of time the pain progressed to left leg up two left feet. She complained of pain and tingling sensation. then she consulted a doctor, who, after various investigations told the patient that her vertebral column (lower back, vertebra-lumbar ) changes were seen and heard. Changes were seen and were kgetting compressed Thus the pain was seen and is radiating to her. Lower back. She was given treatment, along with painkillers. Since then she is consuming painkillers almost daily. She has sleep disturbances (initiation of sleep) due to her lower back pain but is fine once she sleeps. She used to do farming work then, and used to go to the work and daily.
For the next 4 to 5 years, she consulted various doctors to relieve her pain and for better treatment. In this period, she started complaining pain in the upper back (both sides), neck, pain over the face (bilaterally), bilateral eye pain, swollen eyes, headache, tingling, sensation, overhead/scalp, unilateral or bilateral headaches of various intensities , sometimes she complained of having something in her head (she had the sensations) she consulted a neurosurgeon for the said complaints, 10 to 11 years ago, after multiple test, including CT scan done, according to the, OD.
Doctors told them that changes were seen in the CT scan and that some problem was there. And since then she was started on tablet HICALM plus along with her previous medications, for lower back pain. This tablet also help her with her sleep disturbances. She is able to sleep better with that tablet so she started using tablet. HICALM plus daily since 10 to 11 years.
She later consulted various doctors (more than 10) in the last 10 to 15 years as her complaints didn’t subside and no treatment was relieving Herpen totally, and that no doctor was finding the cause. She tried various medications, and she is tensed if she is not taking any medication. If she doesn’t replenish her medications once when over, then she misses taking tablets for few days. She feels tensed and irritable and busters her family to get the tablets as soon as possible.She feels that she needs medicine to live a proper life every day as medicines, relieve her of pain, and she feels better. She stopped working as farmer-made since last five years, due to pains and also financial stability-support given by her children. She does daily chores in her house, self care and hygiene. Maintained . Appetite is normal. She is currently using tablet ETORICOXIB, NEXPRORD, tablet, SULSASALAZINE, tablet HICALM plus,
She can’t sit for long time due to the pain, physical/mental stress. Is increasing her pain sensation. She doesn’t have any relieving factors for her pain other than medications, she constantly thinks about her health, her pains, that she is not able to have a normal life like others, her age due to the pain. She feels low regarding her condition since past 10 years, and she has become less energetic and feels her body has become fragile. She constantly also thinks about her family members, since last 5 to 6 years, she is not able to tolerate loud noises, she gets sick and her pains increase when exposed to loud Noises, no history of head, injury, seizures,
no history of substance, abuse,
no history of hearing of voices, says, talking, self, smiling behaviour,
no history of suicide, ability,
no history of grandiosity, flight of ideas, no history of fear, impending, doom, palpitations,
no history of repetitive thoughts, actions
Past history-
known case of hypertension. Since 10 years uses tablet amlodipine
Family history-
no psychiatric history in the family
On examination
BP-110/70, mmHg
Pulse rate-84 beats per minute
Respiratory rate-19/minutes
Temperature-a febrile
Patient is unable to sit on the chair comfortably for longer duration (more than 10 minutes) due to lower back pain. Patient is moderately built well-kept and responding well to oral commands.
ETEC + and sustained
PMA-normal
Rapport established
RT-normal relevant and coherent
Speech-T ,V,R-normal
Thoughts-constantly things about her pain
Mood-‘dare hai” Lekin accha hai
Effect-Euthymic
Perception-NAD
Oriented to time, place and person
IMPRESSION -1) persistent somatoform disorder in background of physical illness
2)mild depressive episode
PLAN
1. O D. PSYCHO EDUCATED
2. TAB PREGABLIN plus duloxetine, 30 mg.(PREGALIN-D-30).
3. TAB clonazepam 0.25mg/po/(if sleep disturbances present)
4. Stop T. HICALM plus.
Psychiatric follow up (1/05/2023)
Patient is seen complaint on medication took night dose of medication, of medication
Reports to have slept well last night (9:30 PM to 5 AM)
Appetite is normal
No fresh complaints
Patient is sitting on the bed in uncomfortable way as she has back pain. Responding well to oral commands.
ERC +, maintaineded
P M. A-normal
Speech, T, R normal.
R T.-NORMAL, RELEVANT AND COHERENT
THOUGHT-ABOUT HER HEALTH
WORD-‘ACHA HAI’
AFFECT-EUTHYMIC
PERCEPTION, NAD
ORIENTED TO TIME, PLACE, PERSON
1) patient and OD counselled
2) continue medications by neurosurgeon. (gabapentin, duloxetine )
With hold TAB. Pregalin-D.
Psychiatry’s, follow-up notes(2/05/2023)
Patient seen complaint on medication, but took psychiatric medication along with neurosurgery medication (psychiatry, medication was stopped yesterday)
Reports to have slept well last night
Appetite-normal
No fresh complaints
Patient and O D. Strictly counselled to follow treatment accordingly as per plan.
MSE : GAB: patient is sitting on the chair uncomfortably. Due to her back pain, responds well to oral commands.
ETEC +, sustained
P M.A-normal.
Speech-TV R. Normal
RT-normal relevant and coherent
Thought-about her operation Food issue (north, South difference)
Mood-Accha Hai
Affect- Euthymic
Perception-NAD
Psychiatry’s, follow-up notes(3/05/2023)
Patient seen complaint on medication
Took night doors of medication
Report to have slept well last night
Appetite-Normal
No fresh complaints
MSE-patient is sitting on the bed and responding to oral commands
ETEC-present
P M. A-Normal
Speech-TVR-Normal
RT-normal relevant and coherent
Thought-worried about her health
Mood-Accha Hai
Affect- Euthymic
Perception-NAD
Oriented to time, place and person
DISCHARGE SUMMARY
Final diagnosis
DISCHARGE SUMMARY
Final diagnosis
Low backache 15 years
Headache 5 years
IMPRESSION -
1) persistent somatoform disorder in background of physical illness
2)mild depressive episode
3)Hypertension 10 years
patient was married at the age of 18 years ,non consanguineous marriage,she did not receive any form of education ,started working in the farms 4 years after her marriage involving ploughing and sowing ,transplanting the sampling requiring her to bend foward and lean for several hours (5-10hrs/day)
She was apparently asymptomatic 15 years back when she developed low back ache ,which was insidious in onset and gradually progressive , radiating type ,to both the lower limbs more on left side ,more in the calf muscles ,associated with tingling and numbness more the the right side .Pain aggravates on sitting ,she is unable to sit for long durations
PAST HISTORY
K/c/o of Hypertension since 10 years
k/c/o cervical spondylisis since 8 years
COURSE IN HOSPITAL
Patient was investigated further and was found to have persistent somatoform disorder in background of physical illness with mild depressive episode,patient and OD were pyscho educated
Patient was reffered to opthalomogy department to rule out hypertensive retinopathy ,patient didn’t show any signs of following .
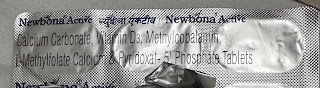
Patient on referral to neurosurgery was prescribed TAB. PREGALIN-D PO/HS (PREGABALIN 75MG+ DULOXITENE 30MG) ,lumbar back support belt
Advice surgery L4-L5 L5-S1 laminectomy and discectomy
patient and OD counselled to continue medications by neurosurgeon. (gabapentin, duloxetine )
Criteria based on AP diameters for lumbar stenosis
https://emedicine.medscape.com/article/344171-overview#a1
The AP diameter of the normal lumbar spinal canal varies widely, from 15 to 27 mm. Lumbar stenosis results from an AP spinal canal diameter of less than 12 mm in some patients; a diameter of 10 mm is definitely stenotic and may be a primary source of symptoms.
Ours patients diameters
L4/L5-11.2 mm
L5/S1-8.6 mm in 2015
Criteria used for surgery requirement
Score more than 7 can be conservatively treated
In our patient
Lower back pain -1
Leg pain or tingling -1
Gait -0
straight leg rasing -1
Sensory loss -2
Motor loss-2
Restrictions of daily activities -1
Bladder function (-3)
1+1+0+1+2+2+1-3= 5
What is the role of Sulfasalazine in rheumatology and why do you think this was given to our patient?
Sulfasalazine is a disease-modifying anti-rheumatic drug (DMARD) that is commonly used in the treatment of rheumatoid arthritis and other inflammatory rheumatic conditions, such as ankylosing spondylitis and psoriatic arthritis. It works by suppressing the activity of the immune system, thereby reducing inflammation and preventing joint damage.
In the case of lower back ache, Sulfasalazine may have been prescribed if the patient is suspected to have an inflammatory condition, such as ankylosing spondylitis or psoriatic arthritis. These conditions can cause inflammation in the joints of the spine, leading to pain and stiffness in the lower back. By suppressing the immune system and reducing inflammation, Sulfasalazine can help to relieve these symptoms and slow the progression of joint damage.
1.What would be a successful treatment for backache? Is the success duration dependent (for example the 2 month success with injection) or is it possible to attain low backache nirvana from surgical interventions?
https://pubmed.ncbi.nlm.nih.gov/30658613/
We analysed 3859 patients with Lumbar Spinal Stenosis [(LSS); mean age 66; female gender 50%] and 617 patients with Lumbar Degenerative Spondylolisthesis [(LDS); mean age 67; 72% female gender]. The accuracy of identifying 'completely recovered' and 'much better' patients was generally high, but lower for EQ-5D than for the other PROMs. For all PROMs the accuracy was lower for the change score than for the follow-up score and the percentage change score, especially among patients with low and high PROM scores at baseline. The optimal threshold for a clinically important outcome was ≤24 for ODI, ≥0.69 for EQ-5D, ≤3 for NRS leg pain, and ≤ 4 for NRS back pain, and, for the percentage change score, ≥30% for ODI, ≥40% for NRS leg pain, and ≥ 33% for NRS back pain. The estimated cut-offs were similar for LSS and for LDS. Conclusion: For estimating a 'success' rate assessed by a PROM, we recommend using the follow-up score or the percentage change score. These scores reflected a clinically important outcome better than the change score. 2.Can you share literature around "failed back pain surgery syndrome"
Failed back pain surgery syndrome (FBPSS) is a term used to describe persistent or recurrent low back pain following spinal surgery. It is a complex and multifactorial condition that can have a significant impact on the quality of life of patients. There are several reasons why surgery may fail, including incorrect diagnosis, inadequate surgical technique, complications during surgery, and underlying medical conditions.
3. randomized controlled trials of trials for discectomy v placebo sham surgery?
https://pubmed.ncbi.nlm.nih.gov/12973134/
Sixty-four patients aged 25-60 years with low back pain lasting longer than 1 year and evidence of disc degeneration at L4-L5 and/or L5-S1 at radiographic examination were randomized to either lumbar fusion with posterior transpedicular screws and postoperative physiotherapy, or cognitive intervention and exercises. The cognitive intervention consisted of a lecture to give the patient an understanding that ordinary physical activity would not harm the disc and a recommendation to use the back and bend it. This was reinforced by three daily physical exercise sessions for 3 weeks. The main outcome measure was the Oswestry Disability Index.
Results: At the 1-year follow-up visit, 97% of the patients, including 6 patients who had either not attended treatment or changed groups, were examined. The Oswestry Disability Index was significantly reduced from 41 to 26 after surgery, compared with 42 to 30 after cognitive intervention and exercises. The mean difference between groups was 2.3 (-6.7 to 11.4) (P = 0.33). Improvements inback pain, use of analgesics, emotional distress, life satisfaction, and return to work were not different. Fear-avoidance beliefs and fingertip-floor distance were reduced more after nonoperative treatment, and lower limb pain was reduced more after surgery. The success rate according to an independent observer was 70% after surgery and 76% after cognitive intervention and exercises. The early complication rate in the surgical group was 18%.















































Comments
Post a Comment